Pulpitis is the inflammation of the dental pulp, typically caused by a bacterial infection. It can result in tooth pain and sensitivity.
Dental health is crucial for overall wellbeing, and understanding conditions like pulpitis is key to maintaining a healthy mouth. Pulpitis emerges when the innermost part of the tooth, known as the pulp, becomes inflamed. This inflammation can stem from various factors such as dental cavities, trauma, or repeated dental procedures.
Affected individuals might experience discomfort ranging from mild to severe, and the condition can be categorized as either reversible or irreversible, dictating the type of treatment required. Early detection and treatment of pulpitis are essential to prevent further complications such as abscesses or tooth loss. Regular dental check-ups and adherence to good oral hygiene practices are the best defenses against such painful inflammation.
Understanding Pulpitis: An Overview
Pulpitis strikes a chord of concern for many. Let’s unravel this dental condition. We’ll explore its definition, dentistry role, and tooth anatomy relation.
Defining Pulpitis: What It Is And Its Relevance In Dentistry
Pulpitis is inflammation of the dental pulp. This is the innermost part of a tooth, where nerves and blood vessels live. It can cause pain and discomfort. It’s crucial in dentistry because it influences oral health status. Timely treatment prevents further complications.
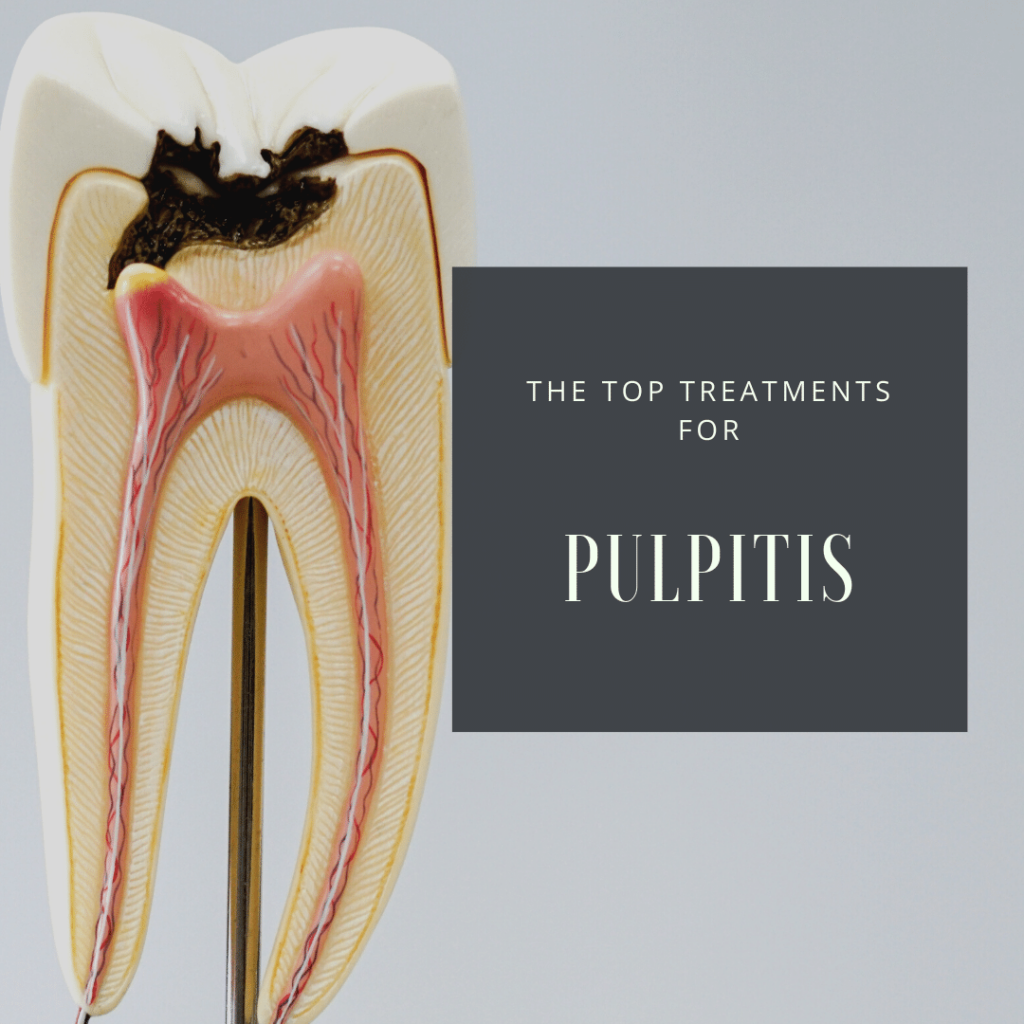
The Anatomy Of A Tooth: Where And How Pulpitis Occurs
Every tooth has layers—the enamel, dentin, and pulp. Pulpitis starts in the pulp chamber. Bacteria or damage triggers it. It can spread to nerves and lead to serious issues.
| Layer | Function | Relation to Pulpitis |
|---|---|---|
| Enamel | Protects tooth | Pulpitis can occur if enamel is breached |
| Dentin | Supports enamel, carries nerve fibers | Bacteria pass through, affecting pulp |
| Pulp | Contains nerves and blood vessels | Directly impacted by pulpitis |
Oral hygiene is key. Brushing and flossing prevent pulpitis risks. Early detection and treatment matter. Regular dental checks help catch issues early. Avoiding pulpitis means healthy teeth and a lasting smile.
Credit: empiredental.ca
The Classifications Of Pulpitis
Imagine your teeth as tiny fortresses, with a soft core known as the pulp. This pulp can get angry and inflamed. This condition is called pulpitis. Pulpitis is a signal your teeth send to tell you something is wrong. It comes in different forms, and knowing the type of pulpitis is crucial. The right treatment depends on the correct type. Let’s explore these types in detail.
Distinguishing Between Reversible And Irreversible Pulpitis
To understand pulpitis, imagine your teeth saying, “I’m in trouble but can fix it,” or “I’m too far gone, help!” This is the difference between reversible and irreversible pulpitis.
- Reversible Pulpitis: This is like a small argument between your teeth and harmful factors. Your tooth responds but can heal with proper care.
- Irreversible Pulpitis: Here, the argument turns into a big fight. The tooth can’t make peace on its own. A dentist must step in to save the day.
Symptomatic Vs. Asymptomatic Pulpitis: Clinical Implications
Pulpitis can be a loud problem or a silent one. Symptoms tell you the pulp is not happy. A lack of symptoms might seem okay, but the problem could still be lurking.
| Symptomatic Pulpitis | Asymptomatic Pulpitis |
|---|---|
| Pain when biting or with hot and cold drinks. Tooth sends clear SOS signals. | No pain, but this does not mean all is well. Hidden issues need a dentist’s eye. |
Symptomatic pulpitis often leads to quicker action. The tooth is asking for help, and you feel it. Asymptomatic pulpitis is sneaky. Regular check-ups catch these silent troubles.
The Causes Of Pulpitis
Understanding what causes pulpitis can help protect your teeth. This condition, where the tooth’s pulp becomes inflamed, leads to pain and discomfort. Let’s explore the common causes of this dental issue.
Dental Caries: A Leading Contributor To Pulpitis
When tooth decay goes untreated, it can lead to pulpitis. Here’s why:
- Bacteria in dental caries produce acids.
- These acids dissolve the enamel, creating cavities.
- As decay reaches deeper layers, it can infect the pulp.
Regular check-ups and good oral hygiene are key preventive measures.
Trauma And Injury: How They Can Lead To Pulpitis
Accidents can damage your teeth. Even a small chip or crack can expose the pulp to bacteria, making it vulnerable:
- Direct hits to the mouth cause trauma.
- Fractured teeth expose the pulp.
- Exposed pulp can become inflamed.
Wearing mouthguards during sports can save your smile.
Iatrogenic Factors: Dental Procedures And Pulpitis
Sometimes, dental work can unintentionally harm the pulp. This is what can happen:
| Procedure | Risk |
|---|---|
| Fillings | Deep fillings can get close to or touch the pulp. |
| Crowns | Prep work might irritate or expose the pulp. |
| Orthodontic Treatment | Adjustments can put stress on the pulp. |
Choose experienced dentists to reduce these risks.
Symptoms And Diagnosis
Pulpitis signals trouble within a tooth, causing distress and discomfort. It strikes when the soft, inner core of a tooth, known as the pulp, becomes inflamed. Spotting the signs early could save your smile. Proper diagnosis is essential for treatment. Let’s explore the symptoms and how dentists pinpoint this common, yet painful, condition.
Recognizing The Symptoms: From Mild Discomfort To Severe Pain
Pulpitis symptoms can vary widely, ranging from barely noticeable to intensely distressing.
- Mild discomfort while eating hot or cold foods
- Toothache that comes and goes
- Constant, severe pain signaling advanced inflammation
- Swelling in nearby gums indicating spreading irritation
Diagnostic Tools And Techniques For Identifying Pulpitis
Dentists have a toolkit to diagnose pulpitis accurately. These are a few ways they achieve this.
- Percussion testing taps on teeth to find tenderness.
- Thermal testing applies heat or cold to detect sensitivity.
- Electric pulp testing checks a tooth’s vitality.
- Examination of past dental records shows the history of the affected tooth.
The Role Of Radiographs In Confirming Pulpitis
Radiographs, or X-rays, are vital in visualizing what’s not visible to the naked eye.
| Type of Radiograph | Purpose |
|---|---|
| Bitewing | Checks for decay between teeth |
| Periapical | Provides a full view of the entire tooth |
| Panoramic | Offers a full mouth view to spot spread of inflammation |
By pairing clinical examinations with radiographic evidence, dentists confirm a diagnosis of pulpitis. This leads to swift and suitable treatment, easing pain and preventing further damage.
Treatment Options For Pulpitis
Pulpitis treatment often depends on the severity and cause of the inflammation. Dentists consider several options to alleviate pain and preserve the tooth. Understanding the range of treatments helps patients prepare for their dental visits.
Conservative Management: When Is It Appropriate?
Treatment for mild pulpitis may include:
- Pain relievers
- Antibiotics, if infection is present
- Reducing tooth load with a temporary crown or onlay
- Careful monitoring over time
Conservative management best suits cases where pulpitis is reversible. Symptoms should subside once the irritant is cleared.
Root Canal Therapy: The Standard Treatment For Irreversible Pulpitis
Irreversible pulpitis often requires more invasive treatment. The process involves:
- Removing the infected pulp
- Cleaning the inner chambers
- Sealing the space with a biocompatible material
Root canals save the tooth while stopping the spread of infection. They offer a high success rate for teeth affected by irreversible pulpitis.
Tooth Extraction: Last Resort In Pulpitis Management
A tooth might be extracted if:
| Condition | Justification |
|---|---|
| Damaged beyond repair | Conservation is not possible |
| Severe infection | Threat to overall health |
| Root canal failure | No other viable treatment |
Tooth extraction is a final step to prevent ongoing pain and complications from severely damaged teeth.

Credit: www.stamforddentalarts.com
Complications And Consequences
Ignoring pulpitis can lead to serious health issues. Teeth are not just for smiling; they play a key role in overall health. Untreated pulpitis may pave the way for complications. It could harm more than just the mouth.
When Pulpitis Is Left Untreated: Potential Risks
Untreated pulpitis is a gamble with dental health. The risks are real and worrying:
- Infection spread: Bacteria can journey from tooth to bone.
- Severe pain: It could go from bad to unbearable.
- Losing teeth: Teeth might say goodbye if pulpitis stays.
- Costly treatment: Delaying care leads to heavier bills later.
Understanding Apical Periodontitis: A Complication Of Pulpitis
Apical periodontitis sneaks in when pulpitis is ignored.
| What Happens? | Consequences |
|---|---|
| bacteria reach the root apex. | It triggers inflammation. |
| Immune system fights back. | Jawbone might get damaged. |
Systemic Implications Of Chronic Pulpitis
Chronic pulpitis isn’t just a tooth issue. It can influence the whole body.
- Heart problems might rise.
- Diabetes control gets tougher.
- Breathing troubles could start.
Keeping teeth healthy helps the entire body stay on track. Don’t let pulpitis take control.
Preventive Measures And Best Practices
Understanding Preventive Measures and Best Practices for pulpitis is essential in maintaining oral health. Pulpitis is the inflammation of the dental pulp, a condition that can cause pain and discomfort. Many cases of pulpitis result from preventable causes. This post will explore actionable strategies to keep your teeth healthy and avoid this painful condition.
Dental Hygiene: A Primary Prevention For Pulpitis
Good dental hygiene is the cornerstone of pulpitis prevention. Daily habits are key. Brushing twice a day with fluoride toothpaste is vital. Remember to floss daily to remove hidden plaque between teeth. Use a soft-bristled toothbrush and replace it every three months. Include a mouthwash in your routine to kill germs.
Here's a simple table on proper brushing technique:
Step Action 1 Apply a pea-sized amount of toothpaste. 2 Hold your brush at a 45-degree angle to gums. 3 Gently move the brush back and forth. 4 Brush inner, outer, and biting surfaces. 5 Finish by brushing your tongue. Regular Dental Check-ups: Early Detection And Prevention
Routine dental visits are crucial for oral health. Dentists can spot signs of pulpitis early on. Experts recommend a check-up every six months. During the visit, your dentist will clean areas your brush can't reach. This can stop pulpitis before it starts.
- Exams can reveal: Cavities, gum disease, and early pulpitis signs.
- Cleanings remove: Hard plaque, potential cause for pulpitis.
- X-rays: Show hidden problems below the gum line.
Diet And Nutrition: Their Role In Preventing Pulpitis
The food you eat affects your teeth. Sugary and acidic foods contribute to tooth decay, a pulpitis risk.
What should you eat?
- Fruits and vegetables
- Whole grains
- Lean proteins
- Dairy products
Avoid snacks like candy and soda. They can harm your teeth. Drinking water helps wash away food particles. It also keeps your saliva levels high, which is good for your teeth.
Remember, prevention is better than cure. These practices will reduce your risk of developing pulpitis and promote overall oral health.
Recent Advances And Research
Recent Advances and Research in pulpitis treatment show promise for better outcomes. With scientific breakthroughs, managing this common dental condition is transforming.
Emerging Treatments For Pulpitis: A Look At The Future
Dental professionals eagerly anticipate new pulpitis therapies. These treatments aim to alleviate pain and save teeth. Here’s a glimpse into what’s on the horizon:
- Biologic medications to reduce inflammation and pain
- Advanced laser therapy that promotes healing
- Nanotechnology-based solutions for precise treatment
The Importance Of Biomarkers In Diagnosing Pulpitis
Diagnosing pulpitis accurately can be challenging. Recent studies focus on biomarkers as a solution. These indicators in our body help identify pulpitis early.
- Genetic markers can signal a predisposition to pulpitis
- Inflammatory biomarkers give clues about the severity
- Molecular flags alert dentists to the exact problem area
Regenerative Endodontics: A New Horizon For Pulpitis Treatment
Regenerative endodontics represents a leap in treating pulpitis. It uses the body’s healing abilities to repair damaged pulp tissue.
- Stem cell therapy to regenerate healthy pulp
- Growth factors encourage the formation of new tissue
- Biocompatible scaffolds provide a structure for tissue growth
Patient Education And Awareness
When it involves dental health, understanding conditions like pulpitis is crucial. Pulpitis, an inflammation of the dental pulp, may cause pain and discomfort. This section educates on timely treatment’s significance, financial considerations, and debunking common misconceptions.
Understanding The Importance Of Timely Treatment
Act fast, avoid complications. Pulpitis doesn’t just go away. Ignoring symptoms may lead to serious issues.
- Prevent infection spread – Timely care stops bacteria from moving to other teeth.
- Save your tooth – Early treatment often saves teeth from extraction.
- Reduce additional treatment need – Quick action limits the procedures needed.
The Financial Cost Of Pulpitis: Insurance And Treatment Options
Pulpitis treatment costs might worry patients. Know your options.
| Treatment | Without Insurance | With Insurance |
|---|---|---|
| Fillings | $50 – $300 | $25 – $150 |
| Root Canals | $300 – $1,500 | $150 – $750 |
| Extractions | $75 – $600 | $37 – $300 |
Always check with your insurance provider. They might cover a significant part. Consider payment plans if you’re uninsured.
Dispelling Myths: Educating Patients About Pulpitis
Myths about pulpitis often scare patients. Let’s clear some up.
- Myth: Pulpitis is always painful
- Not true. Early stages may have no pain.
- Myth: Extraction is the only option
- Pulpitis often gets treated with fillings or root canals, saving the tooth.
- Myth: Painkillers suffice
- They only mask the pain. Treatment is essential.

Credit: www.osmosis.org
Conclusion
Understanding pulpitis is crucial for maintaining dental health. Early intervention can prevent further complications. Regular check-ups and good oral hygiene are your best defenses. If pain or sensitivity arise, consult your dentist promptly. Embrace these practices for a healthy, pain-free smile.

