Periodontitis is a serious gum infection that damages the soft tissue and destroys the bone supporting your teeth. It can lead to tooth loss, and increase the risk of heart attack, stroke, and other health problems.
Periodontitis, often preventable, begins with dental plaque buildup, leading to inflammation of the tissues surrounding the teeth. Without treatment, this condition progresses, forming pockets between teeth and gums, jeopardizing the integrity of the jawbone. Regular dental check-ups, good oral hygiene, and professional cleanings are crucial in preventing periodontitis.
Symptoms may include swollen, red gums, bad breath, and loose teeth. Early detection and treatment by a dental professional can prevent irreversible damage, emphasizing the importance of education and awareness about oral health. Proper management of periodontitis is vital for maintaining overall health and preventing complications.
Understanding Periodontitis
Periodontitis is a common but severe gum disease. It quietly damages the soft tissue and bone that support your teeth. Without knowing, you could lose teeth. This post helps to unwrap the layers of periodontitis, its causes, and effects on oral health.
Definition And Overview Of Periodontal Disease
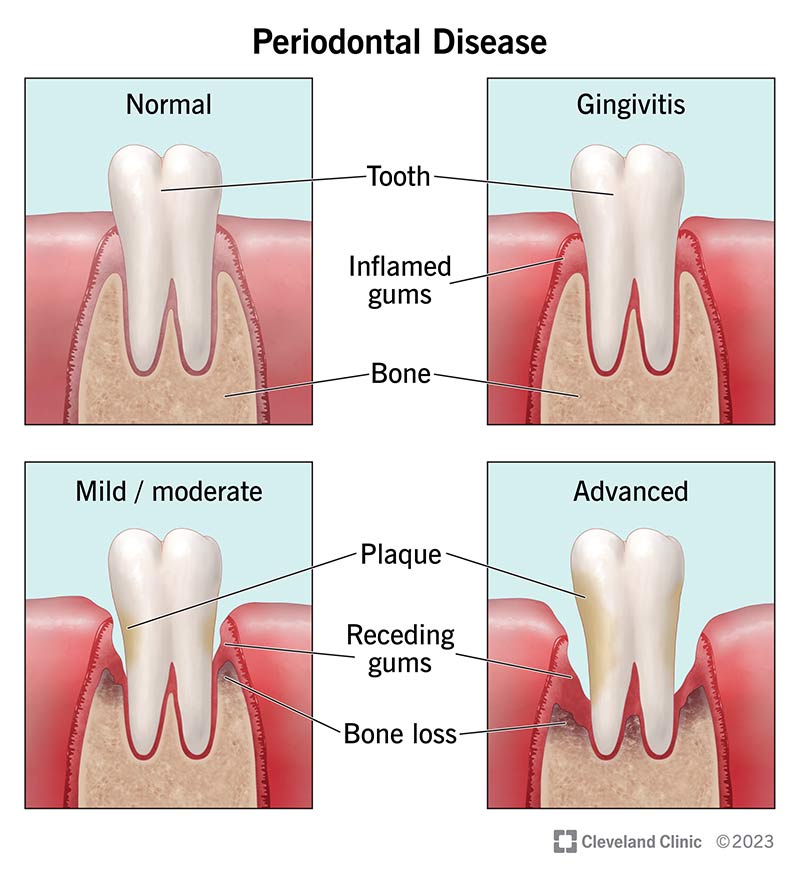
Periodontal disease, also known as gum disease, is an infection of the structures around the teeth. It starts as plaque buildup and can lead to tooth loss. In its early stage, called gingivitis, the gums become swollen and red due to inflammation, which is the body’s natural response to the presence of harmful bacteria.
- Gingivitis is the mild form of periodontal disease.
- Periodontitis is more severe and can damage the bones around your teeth.
- Good oral hygiene can prevent periodontal diseases.
The Pathophysiology Of Periodontitis
Periodontitis begins when the immune system fights against bacteria in plaque. This battle can hurt the surrounding tissues. Over time, deep pockets form between teeth and gums, filled with bacteria and pus. The deeper the pockets, the more damage they cause.
| Stage | Process | Result |
|---|---|---|
| 1. Inflammation | Gums react to bacteria in plaque. | Red, swollen gums that bleed easily. |
| 2. Deepening Pockets | Space forms between teeth and gums. | Collection of bacteria and pus. |
| 3. Tissue Destruction | Immune response damages structures. | Loss of soft tissue and bone, possible tooth loss. |
Knowing the signs of periodontitis is key. They include bleeding gums, bad breath, loose teeth, and receding gums. Early detection and treatment can save teeth and prevent more serious issues.
The Prevalence And Impact Of Periodontitis
Periodontitis is a serious gum infection. It damages soft tissue and can destroy the bone that supports teeth. Without treatment, it can lead to tooth loss and other health problems. It’s common but largely preventable. This condition is typically caused by poor oral hygiene. Brushing at least twice a day, flossing daily, and getting regular dental checkups can greatly improve your chances of successful treatment for periodontitis. It can also reduce your chance of developing it.
Statistical Insight Into Periodontitis Globally
Periodontitis affects many people worldwide. Let’s look at the numbers:
- 743 million people globally have severe periodontitis.
- It’s the 6th most common condition in the world.
- Adults over 30 years have a 47.2% rate of periodontitis.
Economic And Healthcare Burden Of Periodontal Disease
Periodontitis has a big impact on healthcare and economies. Here are some facts:
| Aspect | Impact |
|---|---|
| Treatment costs | High for advanced cases, affecting personal and public healthcare budgets. |
| Work days lost | A significant number due to dental visits or discomfort. |
| Quality of life | Can decrease due to pain, tooth loss, and associated health issues. |
Risk Factors And Causes Of Periodontitis
Understanding the risk factors and causes of Periodontitis is key to prevention and treatment. This severe gum infection can lead to tooth loss if not addressed. Let’s dive into the factors that contribute to its development.
Genetic Predisposition And Periodontal Disease
Your genes can play a big role in your oral health. Some people inherit a higher risk of gum disease. This means even with good oral habits, they must be extra careful to avoid periodontitis.
- Family history of dental diseases increases your risk.
- Genetic tests can sometimes predict susceptibility to periodontitis.
- Regular dental visits are crucial for those at genetic risk.
Environmental And Lifestyle Influences
Your daily habits can affect your risk of developing periodontitis. Smoking, poor nutrition, and stress can all add fuel to the fire when it comes to gum disease.
| Lifestyle Factor | Impact on Periodontal Health |
|---|---|
| Smoking | Increases infection risk and slows healing. |
| Stress | Weakens the body’s immune response to bacteria. |
| Poor nutrition | Limits the body’s disease-fighting capabilities. |
The Role Of Microorganisms In Periodontitis
Gum disease starts when bacteria in plaque build up between your teeth and gums. Inflammation and infection soon follow if left unchecked.
- Plaque forms on teeth daily and must be removed by brushing and flossing.
- Bacteria in plaque release toxins that irritate gums.
- Professional cleanings can keep these harmful bacteria in check.

Credit: www.merckmanuals.com
Symptoms And Diagnosis
Understanding the symptoms and diagnosis of periodontitis is crucial for early detection and treatment. This inflammatory disease affects the tissues that support your teeth. Unchecked, it can lead to tooth loss and other serious health issues. Learn to spot the signs and understand the diagnostic steps you may undergo.
Recognizing The Signs Of Periodontitis
Periodontitis often begins with few symptoms. It might remain unnoticed until it’s serious. Spotting early signs is vital. Here’s what you should watch for:
- Gums that bleed when you brush or floss — a signal of possible infection.
- Gums that are red, swollen, or tender—healthy gums are firm and pale pink.
- Bad breath that doesn’t go away — caused by bacteria in the mouth.
- Receding gums — teeth look longer as gums pull away.
- A change in the way teeth fit together when biting.
- Loose teeth or loss of teeth without any injury.
- Pus between your teeth and gums — sign of an active infection.
Clinical And Diagnostic Procedures For Periodontitis
To diagnose periodontitis, dentists perform specific assessments. Besides checking the symptoms, further tests determine the condition’s severity. Here are common steps:
- Review of medical history: To identify factors that might contribute to symptoms.
- Visual examination: Dentist looks for plaque, tartar, and inflammation.
- Measuring pocket depth: A probe checks for spaces between teeth and gums.
- Dental X-rays: To see if there’s any bone loss.
- Special tests: If the diagnosis is unclear, additional tests might be ordered.
Evaluations often reveal how advanced the periodontitis is. Your dentist will use this information to plan the best treatment.
Prevention Strategies
Periodontitis is a severe gum disease. It can harm gums and destroy the bones that support your teeth. Without care, teeth might loosen or lead to tooth loss. Luckily, you can prevent it. Let’s explore effective strategies to keep your gums healthy and strong.
Oral Hygiene Best Practices
Good oral hygiene starts with daily habits. Here’s how:
- Brush twice a day with fluoride toothpaste for two minutes. Use a soft-bristled brush.
- Floss daily to remove food and plaque between teeth.
- Replace your toothbrush every 3-4 months or sooner if bristles fray.
- Consider using an antibacterial mouthwash to reduce bacteria.
Regular Dental Check-ups And Professional Cleaning
Regular dental visits are key in preventing periodontitis:
- See your dentist at least twice a year for exams.
- Get professional cleanings to remove tartar that can’t be brushed off.
- Talk to your dentist about signs of gum disease to watch for.
Lifestyle Modifications To Prevent Periodontitis
Changing certain habits can lower your risk:
| Lifestyle Factor | Modification |
|---|---|
| Smoking | Quit smoking. It’s a leading cause of periodontitis. |
| Diet | Eat a balanced diet. Choose foods rich in vitamins and minerals. |
| Stress | Manage stress. It can make it harder for your body to fight infection. |
Following these steps can protect your gums from periodontitis. Start applying them today for a healthier smile tomorrow!
Non-surgical Treatment Options
Periodontitis needs attention before it leads to tooth loss. Non-surgical methods can stop this gum disease.
Scaling And Root Planing
Clean deep, protect teeth: Scaling removes tartar. Root planing smoothes roots. Together, they stop disease growth.
- Scaling: Removes plaque and tartar below the gum line.
- Root Planing: Smooths root surfaces, discouraging further tartar buildup.
Antimicrobial Therapy
Fight back against bacteria: Antimicrobial agents target the root cause of infection.
- Rinses to reduce bacteria.
- Antibiotic gels plied beneath the gums.
Adjunctive Therapies: Lasers And Local Antiseptics
Gentle, effective bacteria removal: Lasers offer precision. Antiseptics directly fight germs in gum pockets.
| Laser Therapy | Local Antiseptics |
|---|---|
| Less invasive bacteria targeting. | Applied in deep pockets to reduce bacteria. |
Surgical Interventions
Periodontitis is a serious gum infection that damages gums and can destroy the jawbone. Surgical interventions may become necessary to prevent tooth loss. These surgeries reach deep below the gum line to restore oral health. Let’s explore the types of surgeries used in treating periodontitis.
Flap Surgery For Periodontitis
Flap surgery, also known as pocket reduction surgery, involves lifting the gums back to remove tartar deposits. After deep cleaning, the gums are sutured in place to fit tightly around the tooth. This method reduces the space between the gum and tooth, decreasing the areas where harmful bacteria can grow.
Bone Grafting And Regenerative Procedures
Periodontitis can lead to bone loss. Bone grafting uses fragments of your bone, synthetic bone, or donated bone to replace lost bone. Regenerative procedures may involve the use of membranes, protein grafts or tissue-stimulating proteins to encourage your body’s natural ability to regenerate bone and tissue.
Soft Tissue Grafting And Aesthetic Considerations
Gum recession often accompanies periodontitis. Soft tissue grafting repairs this issue and can improve the look of your smile. The procedure involves taking tissue from the roof of your mouth or using synthetic material to cover exposed tooth roots. This surgery can also enhance gum line symmetry and contribute to a more aesthetic smile.
Advancements In Periodontal Therapy
Advancements in Periodontal Therapy now offer new hope to those suffering from periodontitis. This chronic gum disease wreaks havoc on the supportive structures of our teeth. But recent progress in treatment options is changing the dental landscape. Innovative surgical methods and emerging drug and biological therapies promise better outcomes for patients.
Innovations In Surgical Techniques
The landscape of periodontal surgery is evolving rapidly. Techniques now aim at more than just disease control; they foster tissue regeneration. Patients benefit from reduced discomfort and faster healing times.
- Minimally Invasive Surgery: Smaller cuts mean less pain and swift recovery.
- Guided Tissue Regeneration: Uses barriers to direct the growth of new bone and gum tissue.
- Laser Therapy: High-precision lasers reduce bacteria and promote tissue regeneration.
Emerging Pharmaceuticals And Biological Therapies
Breakthroughs in drug development and biological solutions are setting new standards in periodontal care. These advancements focus on healing diseased tissues and restoring oral health.
| Therapy Type | Benefits |
|---|---|
| Local Antibiotics | Deliver drugs directly to the gums to fight infection. |
| Host Modulation | Adjusts the body’s defense mechanisms to promote healing. |
| Growth Factors | Stimulate tissue repair and regeneration. |
| Gene Therapy | Targets the causes of disease at a molecular level. |
Long-term Management And Prognosis
Long-Term Management and Prognosis of periodontitis involves a commitment to a new level of oral care. Success depends on regular maintenance and vigilance. This condition can be managed effectively with the right approach, potentially reducing the risk of serious health complications.
Maintaining Oral Health Post-treatment
Following successful treatment, a solid daily routine keeps teeth and gums healthy. Brush twice a day with fluoride toothpaste. Floss daily to remove plaque from areas your brush can’t reach. Use mouthwash for an extra layer of protection. Regular dental check-ups and cleanings are non-negotiable. Commit to these steps to guard against the re-emergence of periodontitis.
Monitoring For Recurrence And Secondary Complications
Regular monitoring is crucial to catch any signs of periodontitis returning. Dentists check for gum bleeding, deepening pockets, and bone loss. They will also look out for secondary issues such as gum recession or loose teeth. Skipped appointments could let these go unnoticed. Early detection means prompt treatment, which can have a massive impact on your oral health.
Periodontitis And Systemic Health
Your mouth tells more than the story of your oral hygiene. Periodontitis, a severe gum disease, can signal and affect whole body health.
Link Between Periodontal Disease And Systemic Conditions
Gums infected with periodontitis can open a door to systemic conditions. Bacteria from your mouth enter the bloodstream, potentially affecting other body parts.
- Respiratory issues: Breathed in from the mouth, bacteria can reach the lungs.
- Rheumatoid arthritis: Gum inflammation might worsen joint pain and inflammation.
- Memory decline: Oral bacteria may be linked to conditions like Alzheimer’s disease.
Impact Of Periodontitis On Cardiovascular Health And Diabetes
Cardiovascular Health
Periodontitis and heart diseases share a two-way street. Inflamed gums may increase heart disease risk.
| Periodontitis | Cardiovascular Issues |
|---|---|
| Bacteria in blood vessels | Atherosclerosis |
| Gum inflammation | Increased blood pressure |
Diabetes
For those with diabetes, periodontitis presents a formidable foe. High blood sugar nurtures harmful gum bacteria.
- Gum disease can make blood sugar hard to control.
- Regular cleanings may help keep diabetes in check.
Periodontitis In Special Populations
Periodontitis doesn’t spare any age group. Special populations, including children, adolescents, and the elderly, face unique challenges when it comes to periodontal health. Recognizing the specific needs of these groups helps tailor effective prevention and treatment plans. Let’s explore periodontal health insights and management tips for these diverse age brackets.
Periodontal Health In Children And Adolescents
Good oral hygiene starts young. Children and adolescents may develop periodontal diseases despite their youth. Timely education on dental care is crucial. Here’s how periodontitis can present itself in younger populations:
- Aggressive periodontitis: Rare but rapid, it can affect primary or permanent teeth.
- Chronic gingivitis: Common in children; reversible with good oral care.
For successful prevention, consider these steps:
- Regular dental check-ups to catch early signs.
- Proper brushing and flossing techniques from an early age.
- Nutrition education, stressing low sugar intake to avoid plaque buildup.
Management Of Periodontitis In Elderly Patients
The elderly are at a higher risk for periodontitis due to factors like medications, systemic health issues, and limited dexterity. Management strategies for older adults include:
| Strategy | Benefits |
|---|---|
| Regular dental visits | Professional monitoring and early intervention. |
| Customized oral hygiene tools | Adapted aids for those with mobility issues. |
| Geriatric dental care education | Awareness of unique age-related oral health needs. |
It’s important to consider cognitive impairments that might affect an elderly patient’s ability to maintain oral health routines. Collaborating with caregivers to ensure that dental care remains a priority is essential.
The Role Of Diet And Nutrition In Periodontal Health
The Role of Diet and Nutrition in Periodontal Health is more significant than you might think. What you eat doesn’t just affect your waistline. It’s also crucial for your gums. Poor nutrition can harm your immune system. This increases the risk of encountering gum diseases like periodontitis. A balanced diet, packed with essential nutrients, can help battle infections and improve oral health. Your gums need proper nutrition just as much as any other part of your body.
Nutritional Deficiencies And Periodontal Disease
Let’s dive into how certain nutritional deficiencies make your gums unhappy. Lack of Vitamin C can make gums bleed. Not enough calcium? Your teeth and bones might weaken. Low vitamin D means your body won’t absorb calcium well. And without enough B vitamins, especially folic acid, your gums could become inflamed. Each of these nutrients is like a building block for your gums. Without them, your periodontal health can suffer.
Anti-inflammatory Diets And Their Effects On Periodontitis
Anti-inflammatory diets bring out the big guns against gum disease. Foods high in omega-3 fatty acids do a great job. Think fish, like salmon, and flaxseeds. These foods help reduce inflammation in the body, including your gums. Also, fruits and veggies are heroes for your oral health. They’re packed with antioxidants that fight off the bad guys; we’re talking about bacteria that cause inflammation and lead to periodontitis.
| Food Category | Benefits |
|---|---|
| Fruits and Vegetables | Rich in antioxidants and vitamins |
| Dairy | Provides calcium and vitamin D |
| Fatty Fish and Seeds | Offers omega-3 fatty acids |
Remember, the foods you choose have power. They can protect or pose risks to your gums. Make wise selections to keep your smile bright and healthy.
Interprofessional Collaboration In Periodontal Care
Interprofessional Collaboration in Periodontal Care ensures a comprehensive approach to treating periodontitis. This team-driven strategy combines the expertise of different healthcare providers. Effectively managing periodontal disease often requires more than just dental attention. By working together, health professionals can deliver improved patient outcomes.
The Dentist-hygienist Team Approach
At the core of periodontal care lies the dentist and hygienist partnership. This duo works in tandem to provide thorough periodontal evaluations. They also devise personalized treatment plans aimed at halting the progression of periodontitis.
- Regular Assessments: Identifying signs of periodontal disease early.
- Treatment Execution: The dentist performs restorative procedures while the hygienist focuses on deep cleaning.
- Patient Education: Both provide vital information on maintaining oral health.
Coordinating Care With Other Health Professionals
Periodontal disease links to overall health. Therefore, coordinating care with medical specialists is crucial.
| Health Professional | Role in Periodontal Care |
|---|---|
| Primary Care Physician | Addresses risk factors like diabetes that can worsen periodontal disease. |
| Cardiologist | Assists in managing heart conditions related to periodontal health. |
| Endocrinologist | Helps in controlling hormonal imbalances that may affect gum health. |
In this collaborative environment, clear communication among providers is vital. This ensures that all therapeutic interventions align, enhancing patient care.
Credit: my.clevelandclinic.org
Patient Education And Compliance
Periodontitis is a serious gum disease. It harms the soft tissue. It can destroy the bone that supports your teeth. Without treatment, it can lead to tooth loss. Patient education plays a crucial role in managing this condition. Understanding the disease and following a treatment plan are key. Let’s dive into how to effectively educate patients and ensure they stick to their treatment plans.
Educating Patients On Periodontal Disease
Educating patients is the first step in fighting periodontitis.
What Is Periodontitis?
Periodontitis is an advanced gum infection. It can cause serious problems.
Causes
- Plaque build-up is the main cause.
- Poor oral hygiene leads to plaque hardening under the gum line.
Signs to Watch For
- Red, swollen gums that bleed.
- Bad breath that won’t go away.
- Loose teeth or gum recession.
Prevention Tips
- Brush teeth twice a day with fluoride toothpaste.
- Floss daily to remove plaque.
- Regular dental check-ups are important.
Increasing Patient Adherence To Periodontal Treatment Plans
Once patients know about periodontitis, the next step is sticking to the treatment plan.
Personalized Plans
Each patient gets a unique treatment plan to follow.
Regular Follow-Ups
Regular dental visits help track progress.
At-Home Care
- Daily oral hygiene habits are vital.
- Patients should record their daily activities.
Understanding Risks
Risk factors like smoking can affect treatment success.
Support and Education
Dentists should offer resources and support. Patients can learn more about periodontitis.
Insurance And Costs Related To Periodontitis Treatment
When tackling periodontitis, understanding the financial side is crucial. Treatment costs can add up fast. This is where insurance and other financing options come into play. They can make managing these expenses more manageable for patients.
Understanding Insurance Coverage For Periodontal Therapy
Many dental insurance plans cover periodontal therapy. It’s vital to know what your insurance covers. Basic plans may only cover routine cleanings. More comprehensive plans might handle advanced treatments like scaling and root planing.
- Check your policy details.
- Talk to your insurance provider for specifics.
- Ask your dentist’s office to help with insurance queries.
Preventive care is often covered more than corrective procedures.
Financing And Out-of-pocket Costs For Patients
Treatments for periodontitis can be costly without insurance. Patients might need to consider financing options. Many dental offices offer payment plans to spread out the cost over time.
Look into healthcare credit cards like CareCredit. These can offer no-interest financing if you pay within a certain period. Always read the fine print to understand the terms.
| Treatment Option | Average Cost Without Insurance |
|---|---|
| Scaling and Root Planing | $200 – $400 per quadrant |
| Gum Graft | $600 – $1200 per site |
| Laser Treatment | $1000 – $3000 total |
Remember to ask about all possible out-of-pocket costs before starting treatment. This can include consultations, follow-up visits, and any additional procedures needed. Planning ahead is key to managing your dental health expenses effectively.
Case Studies: Successes And Challenges In Treating Periodontitis
Periodontitis is a severe gum disease. It can lead to tooth loss. Good news—we can treat it. We’ll explore real-life stories. Some showcase triumphs. Others reveal obstacles. Each story teaches us something. Let’s dive into cases and see how success happens and what challenges may come.
Review Of Successful Periodontal Case Management
Some patients beat periodontitis. Their stories inspire us. They followed treatments. They didn’t miss dentist visits. We see a clear pattern:
- Daily oral care matters.
- Regular cleanings make a difference.
- Advanced treatments help.
| Case | Treatment | Outcome |
|---|---|---|
| 1. Jenny M. | Deep cleaning, medication | Gum health restored |
| 2. David P. | Surgery, lifestyle changes | No more bleeding gums |
| 3. Lisa Q. | Laser therapy, education | Keeps all her teeth |
Analyzing Difficult Cases And Lessons Learned
Not all cases are smooth. Some are tough. We have seen failures. We have adjusted methods. What did difficult cases teach us?
- Early diagnosis is key.
- Custom plans are essential.
- Patience is critical.
Look at Chris T.’s case. His periodontitis was advanced. Traditional methods failed. With new approaches, progress was slow. But we learned that persistence pays off. Gradual improvement is still a win.
Maria L.’s condition seemed hopeless. Pockets were deep. Teeth were loose. A tailored plan turned things around. Cutting-edge treatment was used. Patience and dedication worked. Her smile is healthy today. These hard-won successes highlight the resilience of both patients and dental professionals in the face of periodontal disease challenges.
The Psychological And Social Aspects Of Periodontitis
Periodontitis is not just an oral health problem—it goes beyond that. This chronic gum disease affects more than the mouth, spreading its impact to emotional well-being and social life. Understanding these aspects is key for comprehensive care.
The Emotional Toll of Chronic Oral Health IssuesThe Emotional Toll Of Chronic Oral Health Issues
Gum disease can lead to persistent discomfort and worry. This can result in:
- Anxiety about dental health and treatments
- Stress from chronic pain and the potential for tooth loss
- Low self-esteem due to the appearance of teeth and breath
Social Stigma And Quality Of Life Concerns
The effects of periodontitis are felt in social settings.
- People might feel embarrassed to smile or talk closely.
- Concerns about bad breath can lead to withdrawal from conversations.
- Patients may avoid intimate interactions, impacting relationships.
This stigma can lower quality of life and lead to isolation.
Emerging Trends And Future Directions In Periodontology
Periodontitis, a severe gum disease, poses a significant challenge to oral health. Exciting developments in the realm of periodontology promise a future where diagnosis, treatment, and prevention are highly advanced.
Research Frontiers: Gene Therapy and Stem CellsResearch Frontiers: Gene Therapy And Stem Cells
At the cutting edge, scientists explore the regenerative capabilities of gene therapy and stem cells. This approach could redefine periodontal treatment, moving away from traditional methods to ones that could actually rebuild damaged tissues.
- Gene therapy aims to correct defective genes responsible for disease development.
- Stem cells harvested from a patient’s bone marrow or adipose tissue can regenerate lost periodontal structures.
The Potential Of Digital Dentistry And Personalized Medicine
The integration of digital tools in dental practices is transforming patient care. 3D printing and digital imaging enable precise treatments and faster recovery times.
Personalized medicine tailors periodontal therapy to each individual’s genetic makeup, lifestyle, and risk factors. This strategy ensures treatments are more effective and less invasive.
| Tech | Benefits |
|---|---|
| 3D Scanning | Custom implants and precise disease modeling |
| Bioprinting | Tailored tissue scaffolds for regeneration |

Credit: www.merckmanuals.com
Conclusion
Understanding periodontitis is crucial for maintaining oral health. Early intervention can prevent severe complications. Regular dental check-ups and proper hygiene are your best defenses. Remember, a healthy mouth leads to a healthier body. Don’t neglect the signs; take action to preserve your smile and well-being.

