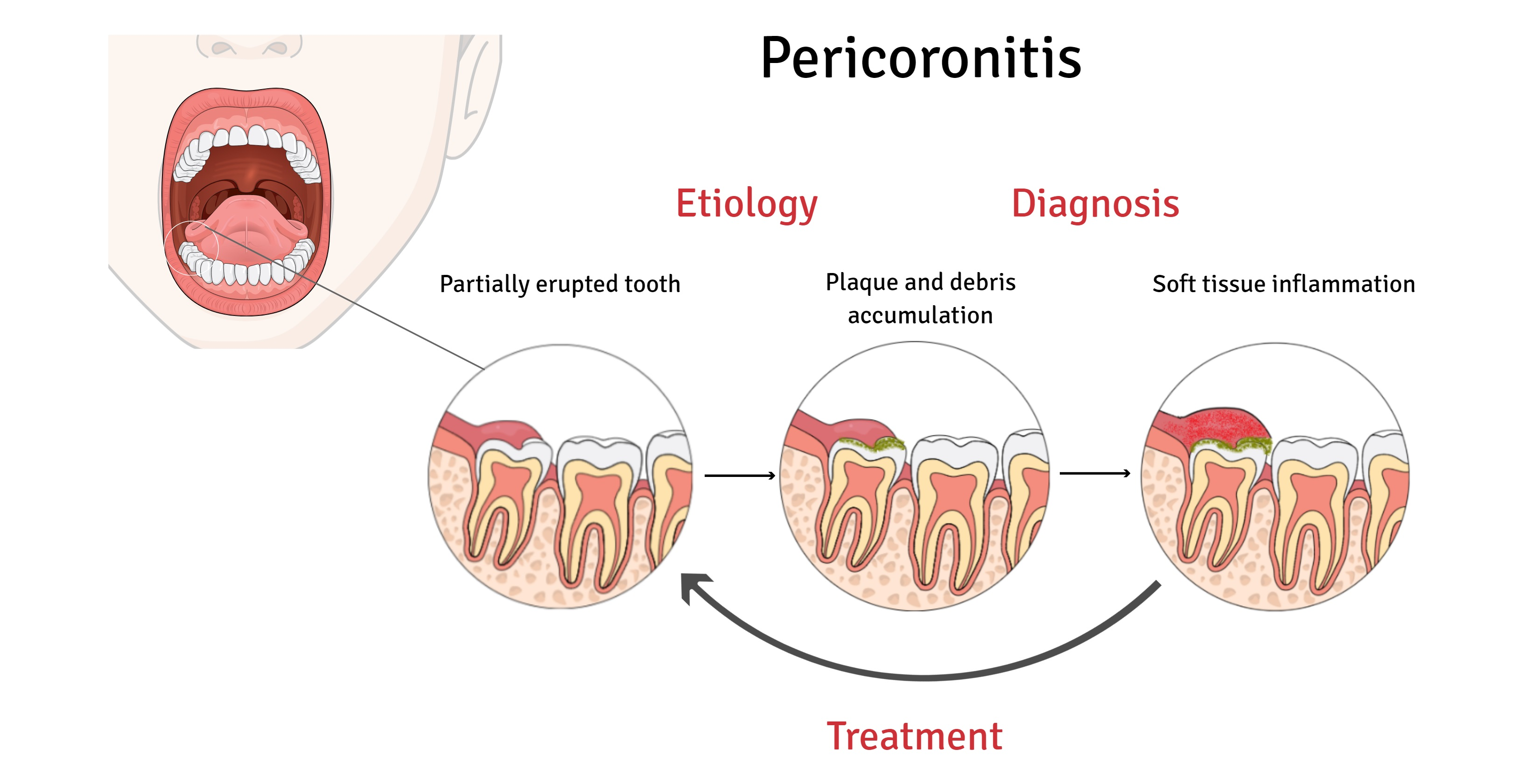
Pericoronitis is an inflammation of the gum tissue around the crown of a partially erupted tooth. This oral condition often affects wisdom teeth that have insufficient space to emerge.
Pericoronitis can be a painful and disruptive dental issue, primarily when it strikes the hard-to-reach area of a wisdom tooth. The condition arises when the partial eruption of a tooth allows bacteria to thrive in the flap of gum covering the tooth, which may lead to swelling, infection, and discomfort.
This inflammation can cause significant pain and, in severe cases, may affect chewing and speaking. Timely dental evaluation and treatment are essential to manage symptoms and prevent complications such as the spread of infection. Good oral hygiene and regular dental check-ups can help minimize the risk of pericoronitis for those with emerging wisdom teeth. Recognizing the symptoms early and seeking prompt dental advice can ensure effective management of this dental condition.
Understanding Pericoronitis: An Overview
Pericoronitis is a dental condition often unnoticed but vital to address. This section dives into what pericoronitis means for your dental health. It affects wisdom teeth as they emerge, leading to discomfort and sometimes serious complications. Read on to grasp the symptoms, diagnosis, and who might be most at risk.
Defining Pericoronitis: Symptoms And Diagnosis
Pericoronitis occurs when the gums around a tooth, usually a wisdom tooth, get inflamed. It can cause:
- Swelling in the affected gum
- Pain that can extend to the jaw and neck
- Difficulty in chewing or opening the mouth
- Bad breath or an unpleasant taste in the mouth
Diagnosis involves a dental examination where a dentist looks for the signs above. X-rays can confirm the condition if needed. If the pain is severe or persistent, seeking dental advice is crucial.
Epidemiology Of Pericoronitis: Who Is At Risk?
Pericoronitis is most common in young adults, typically between the ages of 17 and 24, as this is when wisdom teeth emerge. Factors increasing risk include:
- Poor oral hygiene making it easier for bacteria to cause infection
- Stress which can lead to gum inflammation
- Wisdom teeth that don’t have enough space to grow properly
People with impacted or partially erupted wisdom teeth are especially prone to pericoronitis.
Credit: bestorthodontistbracespune.in
Etiology Of Pericoronitis: Causes And Triggers
Pericoronitis is an unwanted guest that can cause pain and discomfort around your molars. It’s when the gums around your wisdom teeth get swollen and infected. This can happen when a wisdom tooth is not growing into the mouth properly. Knowing what causes this can help prevent it. Let’s look at some common causes and what you can do.
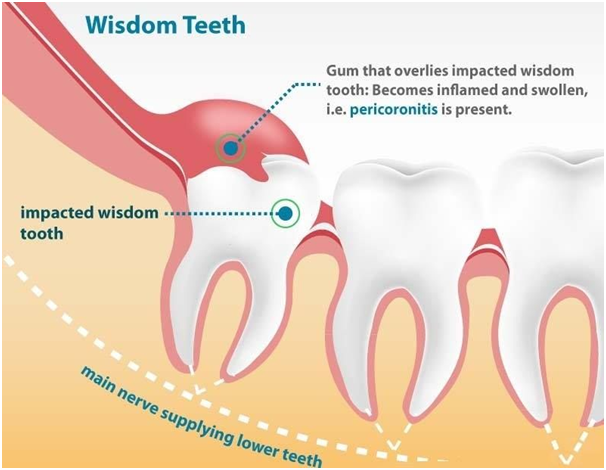
Wisdom Teeth Impaction And Pericoronitis
Wisdom teeth impaction is a big reason for pericoronitis. Such teeth don’t have enough room to grow normally. They can grow at odd angles or not fully break through the gum. This leads to a perfect spot for food and bacteria to hide. The buildup can cause an infection known as pericoronitis. Here are some signs:
- Red, swollen gums
- Pain in the jaw
- A bad taste in your mouth
It’s important to see a dentist if you have these symptoms.
Dental Hygiene And Its Role In Pericoronitis Development
Good dental hygiene can help stop pericoronitis. Bacteria love to stick to teeth and gums, but brushing and flossing can keep them away. If teeth are hard to reach, they’re often not cleaned well. This can lead to an infection. Here’s what you should do to keep your mouth happy:
- Brush twice a day
- Floss daily
- Use mouthwash
If you keep your wisdom teeth area clean, you’ll have a better chance of avoiding pericoronitis. Regular dentist visits are a must too.
Clinical Presentation: Signs And Symptoms Of Pericoronitis
Pericoronitis is an oral health condition that can be painful and disrupt daily life. It occurs when the gum tissue around the wisdom teeth becomes swollen and infected. Recognizing the signs and symptoms early is vital for prompt treatment. This section explores the clinical manifestations of pericoronitis and what to watch out for.
Pain And Discomfort: Recognizing The First Signs
The initial signs of pericoronitis are often pain and discomfort around the affected tooth. This discomfort might be constant or only when you bite down. The pain can also radiate, affecting the ear, jaw, and throat.
- Sore gums: The gum around the tooth is tender
- Difficulty in swallowing: Pain may make swallowing hard
- Bad taste: Possibly due to pus from the infection
- Bad breath: Caused by bacteria in the inflamed area
Inflammation And Infection: Severity Stages
Pericoronitis can progress through several stages, ranging from mild irritation to severe infection. Pay attention to these symptoms:
- Swelling: The gum tissue around the tooth swells noticeably.
- Redness: The area may turn red and feel warm.
- Pus: Infection may lead to pus formation and drainage.
- Fever: A sign the body is fighting an infection.
If any of these symptoms are present, it’s crucial to seek dental advice. Early intervention can prevent complications such as the spread of infection.
Diagnosing Pericoronitis: Methods And Techniques
When discomfort strikes around a wisdom tooth, it could be pericoronitis. This gum condition needs a keen eye to diagnose. Dentists use specific methods to pinpoint pericoronitis. Swift and precise diagnosis leads to effective treatment.
Clinical Examination And Patient History
Your dentist will look inside your mouth. They check for red, swollen gums near a wisdom tooth. Pain and difficulty chewing are key signs. Tell your dentist about your symptoms. Mention how long you have felt them. Share past dental issues too. This history helps in diagnosis.
Radiological Assessment: X-rays And Beyond
Visual checks alone might not tell the whole story. An X-ray gives a clearer picture. It shows how the tooth sits in your jaw. Sometimes, more advanced scans are needed. CT scans help when the situation is complex. They provide 3D views of the tooth and bone.
| Step | Purpose |
|---|---|
| Visual Inspection | Identify visible signs of inflammation |
| Discuss Symptoms | Understand the patient’s experience |
| Dental X-ray | Evaluate tooth positioning and health |
| Advanced Imaging | Gain detailed insight when needed |
- Notice redness or pain? Book a dental visit.
- Keep track of your symptoms.
- Prepare to share your full dental history.
Proper diagnosis of pericoronitis can save your smile. Timely treatment prevents complications. Speak frankly about your discomfort. Trust a dentist to guide your care.
Pericoronitis Treatment Strategies
Battling pericoronitis calls for a strategic approach to alleviate pain and address infection. This section guides you through effective treatment options from the comfort of your home to professional dental interventions, ensuring relief and recovery.
Initial Home Care Remedies And Pain Management
Home care acts as a first line of defense against pericoronitis symptoms. Implement these simple practices to manage discomfort and prevent escalation.
- Rinse with warm salt water gently several times daily.
- Brush using a soft-bristled toothbrush to clean the affected area without causing additional irritation.
- Employ dental floss to dislodge trapped food particles that could aggravate the condition.
- Use over-the-counter pain relievers like ibuprofen to ease inflammation and pain, adhering to the recommended dosage.
Dental Interventions: From Cleaning To Surgery
Should symptoms persist, seek professional dental care. A range of treatments caters to varying severity levels of pericoronitis.
| Severity | Dental Procedure |
|---|---|
| Mild to Moderate |
|
| Severe or Recurrent |
|
Your dentist will determine the best course of action. For severe cases, surgical intervention may become necessary to prevent future episodes of pericoronitis.
Prevention Of Pericoronitis: Proactive Measures
Pericoronitis, a painful oral condition, often lurks unnoticed until it flares up, causing discomfort and potential infection. Combatting this ailment involves a strategic approach to oral health. This segment dives into prevention tactics aimed at maintaining a healthy mouth and warding off pericoronitis.
Importance Of Oral Hygiene And Regular Dental Check-ups
Stellar oral hygiene is your first defense against pericoronitis. A daily routine removes bits of food and plaque that can irritate your gums. Brushing and flossing are the cornerstones of preventing infections.
- Brush your teeth twice a day with fluoride toothpaste.
- Use floss or interdental cleaners daily to reach tricky spots.
- Rinse with an antibacterial mouthwash to reduce bacteria.
Regular dental check-ups detect early signs of pericoronitis. Your dentist can spot trapped food and debris before they cause problems.
- Visit your dentist every six months for a professional cleaning.
- Discuss concerns to catch issues like wisdom teeth impaction early.
Dietary Considerations And Lifestyle Adjustments
| Foods and Habits for a Healthy Mouth | |
|---|---|
| Eat plenty of | Avoid |
| Fruits and vegetables | Sticky, sugary snacks |
| Calcium-rich foods | Hard candies that can damage teeth |
Select foods that strengthen teeth and gums. Limit sugary treats that can lead to plaque buildup.
Lifestyle changes such as quitting smoking improve your oral environment. Smoking increases the risk of pericoronitis.
Potential Complications And Consequences Of Pericoronitis
Pericoronitis is not just a momentary discomfort; it can escalate into serious complications if ignored. This dental condition involves inflammation around a partially erupted tooth, often a wisdom tooth, leading to pain, swelling, and infection. Understanding the potential complications and consequences is crucial for oral health and overall well-being.
Understanding The Risks: From Dental Abscess To Systemic Infection
When pericoronitis is left untreated, it poses several risks:
- Dental Abscess: Pus can collect under the gum, forming an abscess. This can lead to severe pain and requires immediate treatment.
- Spread of Infection: The bacteria causing the infection may spread to the jaw, cheeks, or neck.
- Systemic Infection: In rare cases, the infection can enter the bloodstream, affecting the entire body.
Long-term Effects On Oral Health And Overall Well-being
Ignoring pericoronitis can lead to significant long-term issues:
- Tooth Decay: Trapped food and bacteria can cause cavities in the affected or adjacent teeth.
- Gum Disease: Chronic inflammation can damage gums, leading to gum disease, which might affect other body parts.
- Impact on Overall Health: Poor oral health is linked to heart disease, diabetes, and other health conditions.
Dealing With Chronic Pericoronitis
Chronic Pericoronitis is a mouth problem. It happens around wisdom teeth. Gums can swell and hurt. This post helps you understand how to manage it. We’ll cover regular symptoms and when to take out wisdom teeth.
Management Of Recurrent Symptoms
Pericoronitis gives you sore gums often. Don’t let it control your life. Here’s what to do:
- Rinse your mouth: Use warm salt water. It cleans and eases pain.
- Practice good hygiene: Brush and floss daily. Use a soft, small brush for hard-to-reach places.
- Avoid food traps: Steer clear of popcorn and nuts. They stick in gums and make things worse.
- See your dentist: Regular check-ups help, especially with recurring pain.
When To Consider Wisdom Tooth Extraction
Sometimes taking out wisdom teeth is best. Here’s when:
| Pain Level | Frequency | Impact on Daily Life |
|---|---|---|
| High | Often | Can’t eat or sleep well |
| Medium | Regularly | Work or school affected |
| Low | Sometimes | Minor annoyance |
If the top row fits you, a dentist might suggest extraction. Talk to them about your symptoms. They will say if extraction is the step you need.
Dental Professional Insights: Expert Opinions On Pericoronitis
Pericoronitis is a dental condition. It causes discomfort and swelling around wisdom teeth. Dentists and oral surgeons share their views on its treatment. They use their experiences to help us understand it better.
Dentist And Oral Surgeon Perspectives On Treatment
Experts agree, pericoronitis needs prompt care. They suggest different treatment methods. Below, find the most common solutions they provide:
- Good Oral Hygiene: Brush gently. Use saltwater rinses.
- Medication: Pain relievers and antibiotics often help.
- Operculectomy: Dentists may remove gum flaps.
- Tooth Extraction: Surgeons may take out the affected tooth.
Each case is unique. Dentists weigh the pros and cons. They choose based on the patient’s health.
The Evolution Of Pericoronitis Management
Over time, managing pericoronitis has changed. Thanks to technology and research. Look at the table below for a quick overview.
| Years | Treatment Evolution |
|---|---|
| 1900s | Basic tools, simple extraction methods |
| 2000s | Laser surgery, advanced antibiotics |
| 2020s | 3D imaging, minimally invasive techniques. |
Oral surgeons today have better ways to treat pericoronitis. They ensure patient comfort and quick recovery. Always talk to a dental professional for the best advice.
Credit: www.mdpi.com

Credit: clinicablasi.com
Conclusion
Wrapping up, pericoronitis can be a painful ordeal but is manageable with proper care. Remember to consult your dentist at the first sign of discomfort. Maintaining good oral hygiene and routine check-ups are your best defense against this condition. Take action early to ensure your teeth remain healthy and pericoronitis-free.

